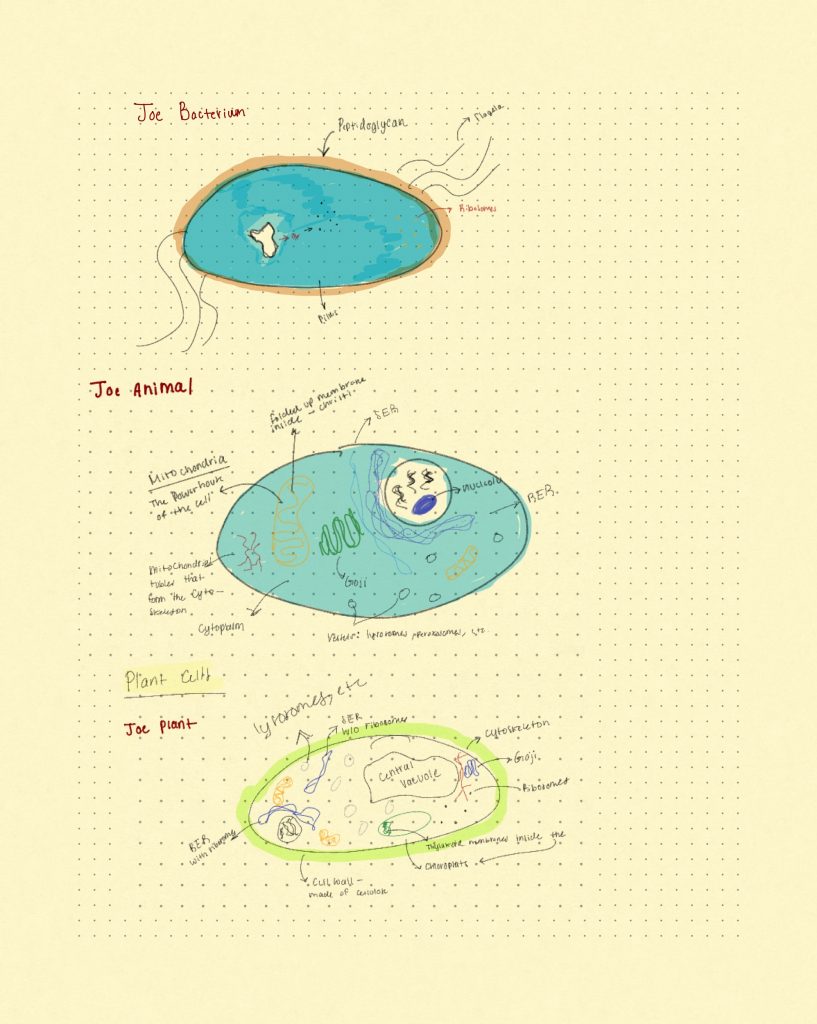
These are my cell sketches!
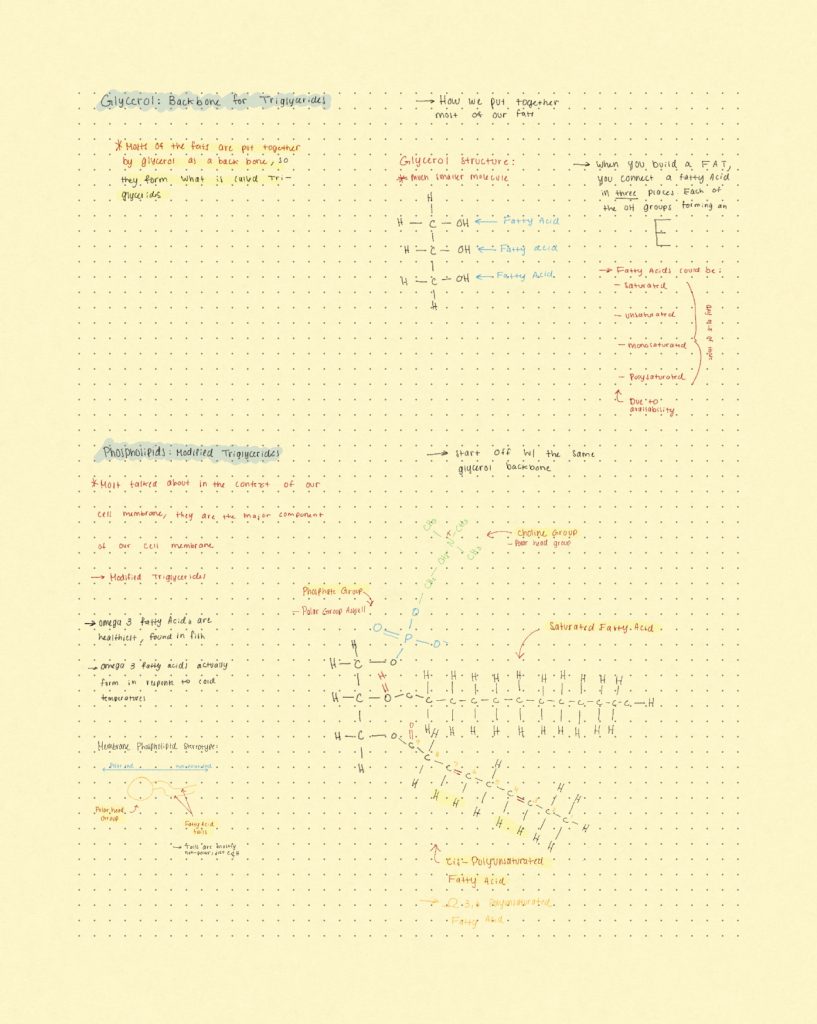
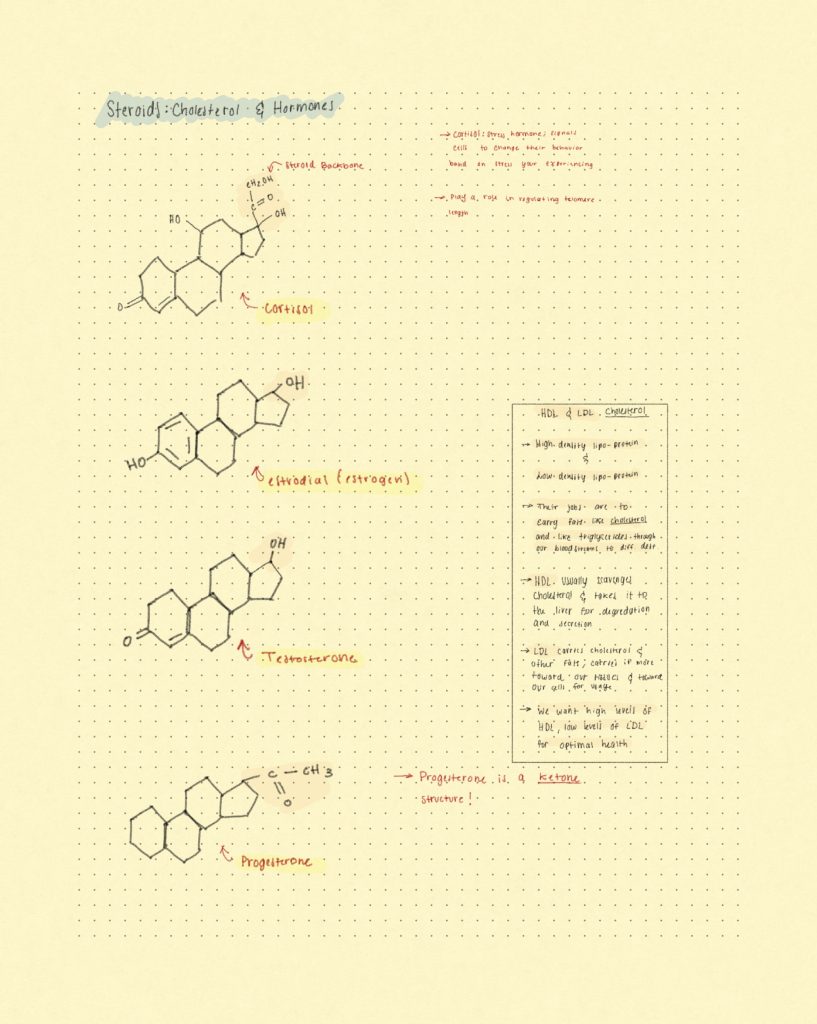
This is an example of a biomolecule: Phospholipids!
Here is my selected meme of the semester!
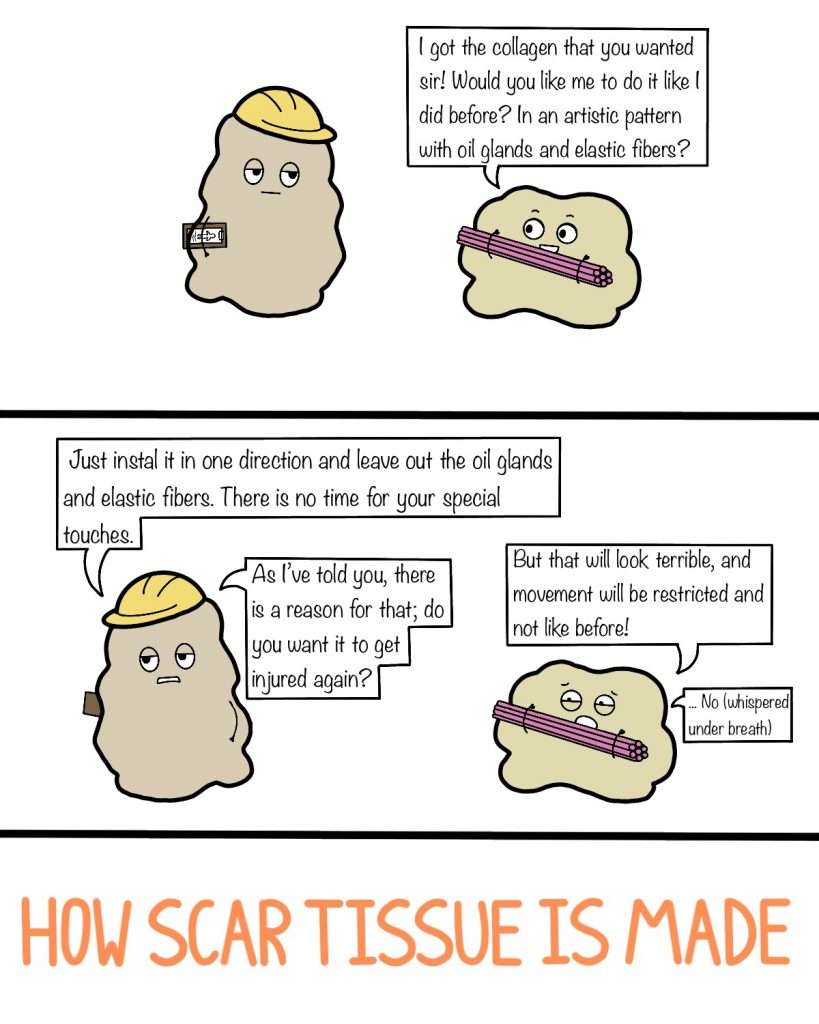
This comic elaborates on how tissue is made: When your body repairs damage, it prioritizes speed over style—collagen is laid down fast without oil glands or flexibility. It protects you, but scar tissue isn’t built to last like the original. The function drops, but the job gets completed.
Scientific Literacy 1: Background Essay
According to the National Heart, Lung, and Blood Institute (NHLBI), cardiac arrest is caused by irregular heart rhythms known as arrhythmias. Risk factors include coronary artery disease, heart failure, arrhythmias, and inherited disorders such as long QT syndrome. Cardiac arrest is frequently fatal, with survival rates around 8%. In 2019, there were about 232,000 emergency department visits in the U.S. involving cardiac arrest, making up roughly 0.2% of all ED visits. Older adults, men, Black individuals, those with lower household incomes, and people visiting the ED on weekends had a higher likelihood of experiencing cardiac arrest. Additionally, those with Medicare insurance and visits in the fall or winter months were at a greater risk. Hispanic individuals, on the other hand, had a lower risk of cardiac arrest in the ED. Certain health conditions, like diabetes and cancer, along with trauma centers, hospitals in metropolitan areas or those with teaching programs, and hospitals located in the South, were linked to higher rates of ED cardiac arrest. On the other hand, conditions such as depression, dementia, and hypothyroidism were associated with a lower risk. The most common causes of cardiac arrest in the ED included septicemia, heart attacks, and respiratory failure, with drug overdoses also contributing significantly.
In addition to these risk factors, the NHLBI emphasizes that heavy alcohol use, intense physical exertion, and the use of substances such as cocaine, amphetamines, and marijuana increase the possibility of cardiac arrest. Excessive caffeine intake, specifically from powders, pills, or energy drinks, is also related to heightened risk, with recommendations suggesting no more than six 5-ounce cups of coffee daily. Severe emotional stress and current influenza infections have also been associated with increased chances of cardiac arrest. Additionally, while sudden cardiac arrest may occur after physical activity, regular exercise is beneficial and helps lower the overall risk.
Ischemia/reperfusion injury refers to the tissue damage that happens when blood supply returns to tissue after a period of ischemia or deficiency of oxygen. While restoring blood flow is crucial to prevent irreversible tissue damage, the process of reperfusion can paradoxically worsen cellular dysfunction and cause cell death. This injury mechanism is involved in various organs, including the heart, lungs, kidneys, gut, skeletal muscle, and brain, and can contribute to multi-organ failure.
Intercellular mitochondrial transfer involves moving healthy mitochondria from one cell to another, potentially improving mitochondrial function in cells with dysfunction. Mitochondrial transplantation, the deliberate transfer of healthy mitochondria into damaged cells, could treat mitochondrial diseases by altering the mitochondrial DNA in affected cells. While it appears to be promising, challenges such as integration and immune rejection delay its widespread medical use.
Scientific Literacy 2: Data Analysis
Mitochondrial transplantation (MTx) may benefit ischemia-reperfusion (I/R) injury following cardiac arrest (CA). In Hayashida et al. (2023), scientists investigated whether one could effectively transplant donated mitochondria into neural cells, the level of function on transplantation, and the therapeutic effects of MTx on survival and physiological recovery following CA.
To begin, the authors established that mitochondria from the donor rat brain and pectoral muscles were easily internalized into neural cells when in vitro cultured. They observed co-localization of exogenous and endogenous mitochondria with neural cells within 24 hours of co-culture through fluorescent molecule labeling. It was indicative of successful incorporation and internalization. Function was established by ATP content and mitochondrial membrane potential measurement, which were much higher in freshly isolated mitochondria compared to frozen-thawed samples. Bioenergetic activity was seen in freshly isolated mitochondria, validating that they were viable after transplantation.
In a cardiac arrest model in a rat, intravenous infusion of freshly isolated mitochondria following resuscitation led to spectacularly improved survival and post-arrest health indicators. Survival was enhanced from 54.5% in the control group to 90.9% in the mitochondrial transplant group. Neurofunction, as measured by a neurofunctional scoring system, was significantly enhanced in treated rats. The mitochondrial transplant group also had better metabolic recovery: arterial lactate and glucose levels normalized sooner, pH stabilized sooner, and carbon dioxide levels decreased sooner than in control groups. Cerebral perfusion was also significantly restored, as treated rats restored cerebral blood flow levels higher than baseline at two hours of resuscitation. Lung edema also decreased substantially, as treated rats showed healthier body weight during the recovery phase of 72 hours.
The study also addressed whether transplanted mitochondria persisted in tissues. Donor mitochondria were detected by confocal microscopy within the brain, kidney, and spleen 24 hours after injection, demonstrating that mitochondria not only penetrate target organs but also persist for at least one day after infusion. No significant persistence was observed in the heart, liver, or lungs after 24 hours, which may reflect tissue-specific uptake or clearance mechanisms.
Surprisingly, the authors demonstrated that frozen-thawed mitochondria were lacking in therapeutic potential. Frozen mitochondria had extremely low amounts of ATP and membrane potential, indicating loss of function. Animals treated with frozen mitochondria showed no enhancement of survival or physiological markers. This demonstrates the very important necessity of using fresh functional mitochondria in transplantation therapies to ensure bioenergetic and therapeutic effectiveness.
Lastly, the findings of Hayashida et al. (2023) indicate that mitochondrial transplantation can successfully deliver functional mitochondria into neurons and enhance survival and recovery in a post-cardiac arrest scenario to a large degree. The study emphasizes the need for using fresh mitochondria, as only respiring, intact mitochondria were found to be able to exert protective effects. The findings open a positive stage for future research on MTx as a novel therapeutic intervention for ischemic damage.
Reference:
Hayashida, K., Takegawa, R., Endo, Y., Yin, T., Choudhary, R. C., Aoki, T., Nishikimi, M., Murao, A., Nakamura, E., Shoaib, M., Kuschner, C., Miyara, S. J., Kim, J., Shinozaki, K., Wang, P., & Becker, L. B. (2023). Exogenous mitochondrial transplantation improves survival and neurological outcomes after resuscitation from cardiac arrest. BMC Medicine, 21(56). https://doi.org/10.1186/s12916-023-02759-0
End-of-term reflection!
One thing I learned in this cell biology class that really helped me make a connection to my other coursework was understanding how G-protein coupled receptors (GPCRs) work in cell signaling. I first really understood this topic while posting discussion responses on PackBack, where I researched how GPCRs are involved in common medications. As someone who wants to become a Physician Assistant, it made me realize how important it is to know exactly how drugs interact with the body at the cellular level. This helped me connect what I was learning in cell biology to my future work in pharmacology and patient care. It also made me a stronger student because I started thinking about biology topics in a more applied and clinical way, not just memorizing information for exams.


Leave a Reply