Find Me a -mAb: Abciximab
Abciximab is a monoclonal antibody that is used as a drug to treat patients who have suffered from an ischemic stroke or myocardial infarction as an antithrombic agent. Abciximab can also be used to treat unstable angina because angina can cause plaque to rupture, which would lead to the aggregation of platelets, ultimately causing a thrombus (2). Gralla et al (2008) performed a study in which abciximab was used to treat patients who had suffered from an ischemic stroke. In this study, about sixty-eight percent of patients who received this drug had their obstruction completely resolved. About twenty percent of the patients in the study had a partial resolution of the thrombus (3). Sengottuvelo and Sekar (2013) performed a study using abciximab in STEMI patients. In all of the patients in this study, an increase in cardiac blood flow was observed to varying degrees (5). This drug works by interrupting platelet aggregation which decreases the ability of blood to clot. The administration of abciximab is usually paired with the administration of Heparin to prevent hemorrhage in the patients. Another risk of the use of abciximab is thrombocytopenia, which is a platelet deficiency; however, this is not a common issue among patients who receive abciximab (2). The optimal conditions to minimize bleeding risks while administering abciximab is still under review. A combination of many factors including the prolonged administration of heparin and an undetermined minimal dose necessary for effective treatment increase the risk of complications in clinical settings (6). The use of abciximab as an antithrombic agent could save many lives as it is used to treat two of the deadliest conditions.
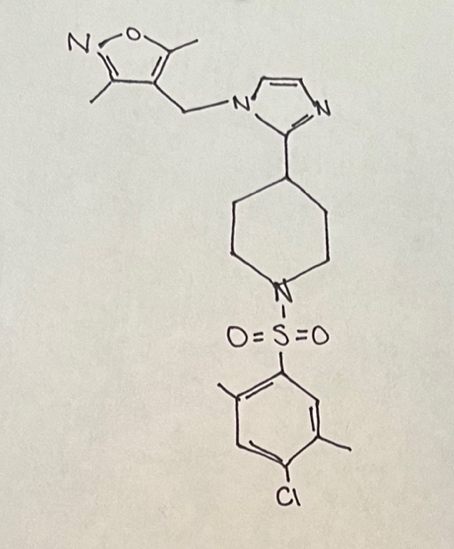
Abciximab is part of the IgG class of antibodies (1). Below is sketched the chemical structure of abciximab as found on chemspider.com (4).
Abciximab is thought to bind to platelet GP IIb/IIIa receptors. This drug works by inhibiting the formation of cross-links among platelets which prevents platelet aggregation. This plays a key role in treating conditions such as an ischemic stroke or a STEMI because these diseases are caused by a blood clot. If the platelets are not allowed to aggregate, the possibility of a blood clot forming and remaining in the vessel is very low (5). Abciximab is only able to treat ischemic strokes because these are caused by a loss of blood flow due to a blood clot. On the other hand, abciximab would be detrimental to a patient experiencing a hemorrhagic stroke because these are caused by excessive bleeding in the brain instead of a thrombus (3). A STEMI is caused by a blood clot in one or multiple vessels in the heart. In STEMI pateints, the use of Abciximab can be used to prevent platelet aggregation which leads to the dissolution of the thrombus in the heart. Ideally, blood flow would be returned to most or all of the heart after this treatment. Once blood flow can be returned to the respective areas, whether it is the brain or the heart, the continued damage due to ischemia will be prevented. The interruption of blood flow can lead to tissue death if it occurs for a long period of time. The use of abciximab as an antithrombic agent has the potential to minimize tissue damage and tissue death due to its ability to prevent the aggregation of platelets (5).
References
- Curtis, B. R., Civgi, A., Garrity, M., & Aster, R. H. (2004). Delayed thrombocytopenia after treatment with abciximab: A distinct clinical entity associated with the immune response to the drug. Journal of Thrombosis and Haemostasis, 2(6). 985-992. https://doi-org.proxy.lib.odu.edu/10.1111/j.1538-7836.2004.00744.x
- Drewe, E. & Powell, R. J. (2002). Clinically useful monoclonal antibodies in treatment. Journal of Clinical Pathology, 55(2). 81-85. DOI: 10.1136/jcp.55.2.81
- Gralla, J. et al (2008). Abciximab for thrombolysis during intracranial aneurysm coiling. Neuroradiology, 50(12). 1041-1047. DOI: 10.1007/s00234-008-0457-8
- Royal Society of Chemistry. Abciximab. https://www.chemspider.com/Chemical-Structure.3041712.html#
- Sengottuvelu, G. & Sekar, V. R. (2013). Intracoronary abciximab in STEMI using local drug delivery catheter – Single center experience. Indian Heart Journal, 65(3). 256-259. https://doi.org/10.1016/j.ihj.2013.04.021
- Windsetter, U., Huber, K., & Gulba, D. C. (1997). New antithrombotic agents: An overview. Fibrinolysis and Proteolysis, 11(1). 85-96. https://doi.org/10.1016/S0268-9499(97)80030-6
